Podcast
Alert on Surgical Items Left Behind in Patients
Dec 29, 2023
“We were aware that best practices had been published, but given the continuing occurrence of these events, thought that there might be some barriers or ongoing challenges.”
Yvonne Cheung, MD, MPH, MBA
Associate Medical Director, AMC PSO
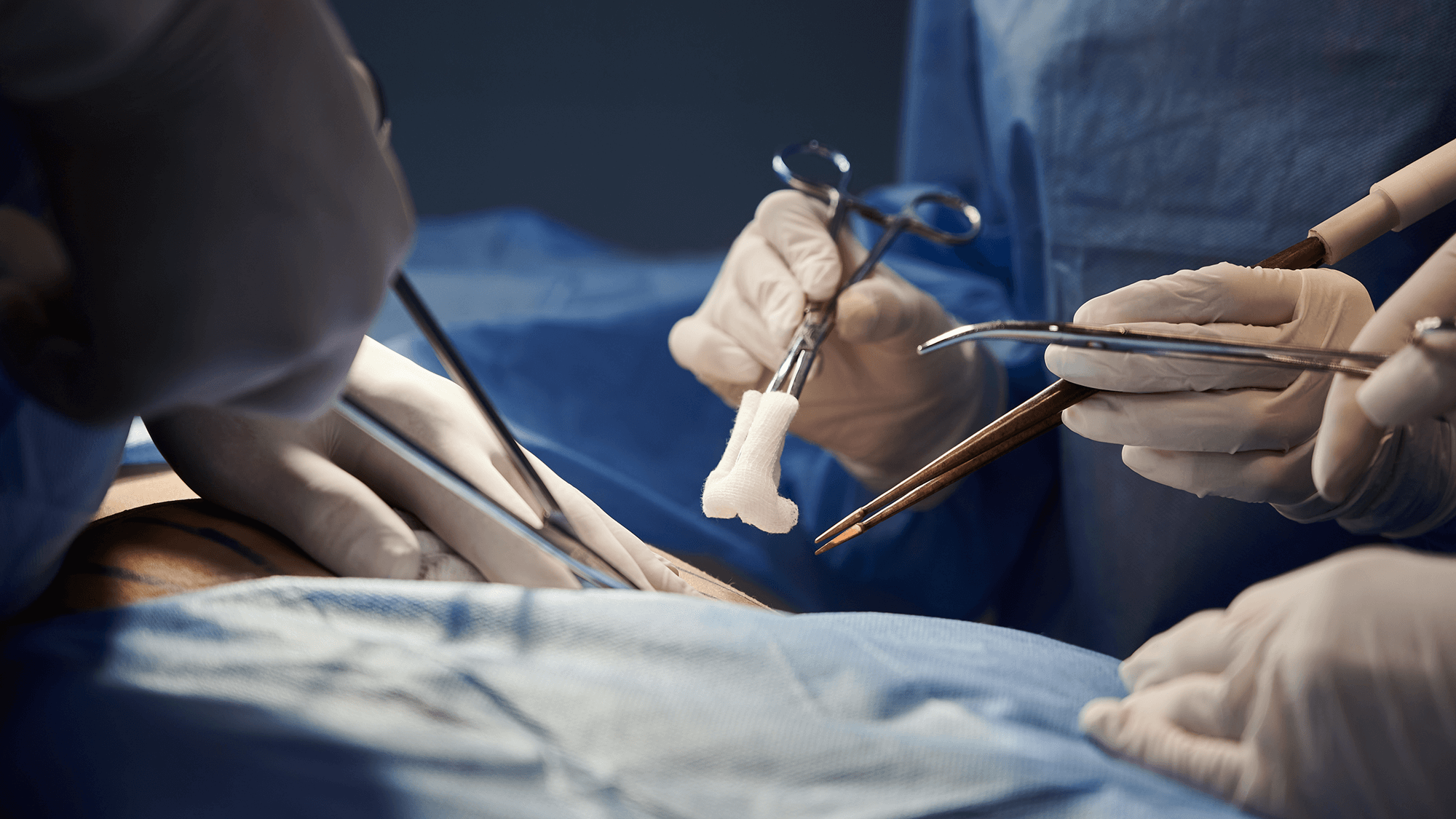
A retained surgical item is patient safety lingo for when a surgical team leaves something like a sponge or a tool inside the patient after surgery. These events may lead to serious harm, such as sepsis, prolonged hospitalization, the need for subsequent surgery, or even death. In late 2023, the Academic Medical Center Patient Safety Organization, or AMC PSO, issued an advisory noting a spike in reports of retained surgical items. The Joint Commission calls them never events, and it’s been a long-term challenge for operating rooms.
“Well, it’s defined as a never event. I must admit I personally have a hard time with that term. When human beings are involved, it’s hard to make things never events.”
Dr. Douglas Smink is a general surgeon at Brigham and Women’s Hospital in Boston and was an advisor for the PSO alert on retained surgical items. The group found varied data showing that these events are persistent and growing, despite known effective interventions. According to the Massachusetts Department of Health, for example, in 2022 the number of serious reportable events involving retained surgical items was 42, an increase to pre-pandemic levels. ‘Retained items’ is the top surgical category for two years in a row in that state.
“I wouldn’t call them common, but they’re more common than some of the other patient safety events that we also are concerned about in the OR, and common enough that we thought it was worth bringing a group together to try to shed some light on them and bring some awareness, but also bring some expertise around how we can try to reduce the reduce the risk, because the main reason is this is a risk to patients.”
A main task for the PSO was to identify key barriers to implementing effective strategies that help prevent retained surgical items. Dr. Yvonne Cheung is an anesthesiologist and Associate Medical Director of the AMC PSO who co-authored the alert. Dr. Cheung said PSO members own data indicated an on-going problem that might suggest impediments to improving.
“We were aware that best practices had been published, but given the continuing occurrence of these events, thought that there might be some barriers or ongoing challenges and thought that was worth convening subject matter experts to really think about the patient safety risks and develop risk mitigation strategies specifically focused on operationalizing best practice guidance.”
The team identified three main risks to preventing retained surgical items:
- Distractions,
- Handoffs, and
- Problems with relationships and trust.
“You know, I think that they are all equally important, but simply by numbers, I would say probably distraction is a higher number because there are more distractions or potential distractions in any kind of procedure versus handoffs tend to happen less frequently unless the procedure and duration is prolonged. And then the third one, relationships and trust is sort of an all-encompassing, not unique to any one organization, but basically, it’s related to opportunities to improve psychological safety and therefore improve the effectiveness of any kind of team that’s working together.”
This last risk is hard to solve with a checklist. The Patient Safety Alert describes a hypothetical case study assembled from multiple real malpractice cases. It involves a 60-year-old patient with multiple co-morbidities, who was admitted for elective exploratory laparotomy. Prior to closure of the skin, the surgical services staff identified one less sponge than expected during the count. The surgeon was notified but continued with closing the wound. Later X-ray revealed the sponge in the patient’s abdomen and another surgery was required to remove it.
Important interventions for trust and safe environments involve establishing team structures with clear roles that empower someone to stop activity to count items. Team training and simulation with closed loop communication and simulated crew resource management are part of effective prevention.
“Unless we really train everyone to respond positively to any kind of raising of hands and accept that there will be some false positives, that someone is going to raise their hand and it’s actually going to be okay, we still need to thank that person just as if it was a true positive and they actually identified something that was truly not what was intended. I think we just have farther to go in terms of that work, sort of positive reinforcement regardless of whether or not it was a true or false positive.”
Standardized and structured hand-offs will help mitigate the other serious risks to safety: shift changes and distractions. Shift changes during counts are discouraged. Raising awareness for the entire team can help. Dr. Smink notes that knowing what is behind a general barrier like distraction allows hospitals to focus on specific factors. Environmental distractions might include noise, side conversations, electronic devices, or patient charting. According to Dr. Smink, a careful count requires the whole team’s attention.
“That count at the end in particular is at a somewhat busy time for the rest of the operating room team. The surgeons are often finishing the procedure, but they’re doing a lot of sewing or other things to put the incision back together. The anesthesiologists are thinking about waking the patient up, and at that same time, usually the circulating nurse and the scrub tech or the scrub nurse are doing the count. But sometimes they’re being distracted because they’re asked for pieces of equipment or something that either the surgeon or the anesthesiologist might need. And those distractions make it hard to count.”
The PSO alert includes a number of suggestions to mitigate distraction during the count, such as addressing the surgeon by name to verify they are ready. Announcing to the entire room that the count is beginning is another recommendation, along with setting up a “no-interruption zone” to create a distraction-free time.
A more expensive but effective intervention is the universal use of bar code wands for institutions that can afford them. Dr. Cheung:
“They will catch the errors when the count was correct and be more facile in detecting where the sponge might be, whether the count is correct or not correct. So that’s one possibility and then I think the second one, in particular for those institutions that may not be able to implement the wanding is to recognize that these events happen; they are preventable; and to understand and work on the other factors, meaning reducing distractions that may or may not be necessary, focusing on reliable, highly reliable handoffs in transitions of care. And then doing whatever we can to optimize psychological safety, not just in the procedural areas but actually in any sort of health care situation or care setting, so that everyone truly feels like they are a valued member of the team and that they feel comfortable speaking up anytime they are not sure that everything is right—not just when they are sure something is wrong—anytime they are not sure everything is right.”
The AMC PSO Patient Safety Alert, Guidance to Reduce the Risk of Retained Surgical Items is available free of charge on the CRICO web site, at www.rmf.harvard.edu/retainedsurgicalitems.
I’m Tom Augello for Safety Net.
Commentators
- Yvonne Cheung, MD, MPH, MBA
- Douglas Smink, MD, MPH
About the Series
We’ve got you.
Our Safety Net podcast features clinical and patient safety leaders from Harvard and around the world, bringing you the knowledge you need for safer patient care.
Episodes
Teleradiology Leads Virtual Care Risk in New Study
New Study Finds Outpatient Adverse Events Common, Often Preventable

Taking the Pulse of a Clinician’s Interpersonal Skills

Bringing AI Into Medicine and Keeping It Safe


